Pre-Existing Chronic Heart Failure in Kidney Transplantation: An Underestimated Risk Factor for Graft Loss?
F. Halleck, D. Khadzhynov, L. Lehner, E. Schrezenmeier, M. Duerr, A. Kleinsteuber, K. Budde, O. Staeck.
Nephrology, Charité
University, Berlin, Germany.
Meeting: 2016 American Transplant Congress
Abstract number: B216
Keywords: Heart failure, Kidney transplantation, Outcome
Session Information
Session Name: Poster Session B: Kidney: Cardiovascular and Metabolic
Session Type: Poster Session
Date: Sunday, June 12, 2016
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Halls C&D
BACKGROUND: Cardio-renal interactions influence graft and patient survival in kidney transplant recipients (KTR). There is only few data available analyzing pre-existing chronic heart failure (CHF) on long-term outcomes after kidney transplantation.
METHODS: This retrospective single center observational study included 878 adult deceased donor KTR transplanted from 1999-2014. Prevalence of comorbidities was determined at time of transplantation. 69 patients with pre-existing systolic or diastolic CHF diagnosed by echocardiography were identified. Follow-up analysis included survival, graft function determined by imputed cGFR (MDRD formula) and graft survival up to 15 years.
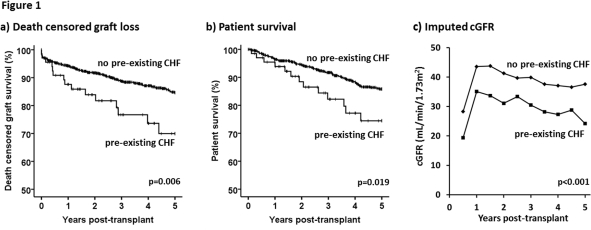
RESULTS: Mean follow-up in the cohort was 5.8±3.8 years. Mean age and donor age were 53±14 and 54±16 years, respectively. KTR with pre-existing CHF were significantly older, had higher donor age and higher prevalence of coronary artery disease (CAD). Gender, time on dialysis, number of previous transplants, diabetes, cold ischemic time and HLA-mismatches did not differ significantly. KTR with pre-existing CHF had a significantly reduced graft (70 vs. 85%, p=0.006) and patient survival (74 vs. 86%, p=0.019) at 5 years post-transplant (Fig. 1 a,b). cGFR was significantly lower (24 vs. 38 ml/min at 5 yrs; p<0.001; Fig1c). Multivariate cox regression analysis revealed CHF as an independent predictor for graft loss (HR 2.31, p<0.001). Other independent risk factors were donor age and HLA mismatches. Pre-existing diabetes or CAD did not contribute independently as risk factors for graft loss. Further analyzing the incidence of post-transplant immunologic events in an adjusted model confirmed that TCMR (HR 2.25; p<0.001), de novo DSA (HR 2.48; p<0.001) and ABMR (HR 1.90; p=0.005) also independently added risk for graft loss to a comparable degree as pre-existing CHF.
CONCLUSION: Pre-existing CHF is not only associated with increased mortality but also a strong independent risk factor for deterioration of renal function and graft loss. This emphasizes the need for thorough pre-transplant evaluation and consequent treatment of CHF.
CITATION INFORMATION: Halleck F, Khadzhynov D, Lehner L, Schrezenmeier E, Duerr M, Kleinsteuber A, Budde K, Staeck O. Pre-Existing Chronic Heart Failure in Kidney Transplantation: An Underestimated Risk Factor for Graft Loss? Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Halleck F, Khadzhynov D, Lehner L, Schrezenmeier E, Duerr M, Kleinsteuber A, Budde K, Staeck O. Pre-Existing Chronic Heart Failure in Kidney Transplantation: An Underestimated Risk Factor for Graft Loss? [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/pre-existing-chronic-heart-failure-in-kidney-transplantation-an-underestimated-risk-factor-for-graft-loss/. Accessed February 5, 2026.« Back to 2016 American Transplant Congress
